Your message has been sent.
 CLOSE SIDEBAR
CLOSE SIDEBAR
Characterizing Blood Transfusion on Distal Aortic Blood Flow During Supra-Celiac Complete Aortic Occlusion in Swine Model
Hisham I. Qadri
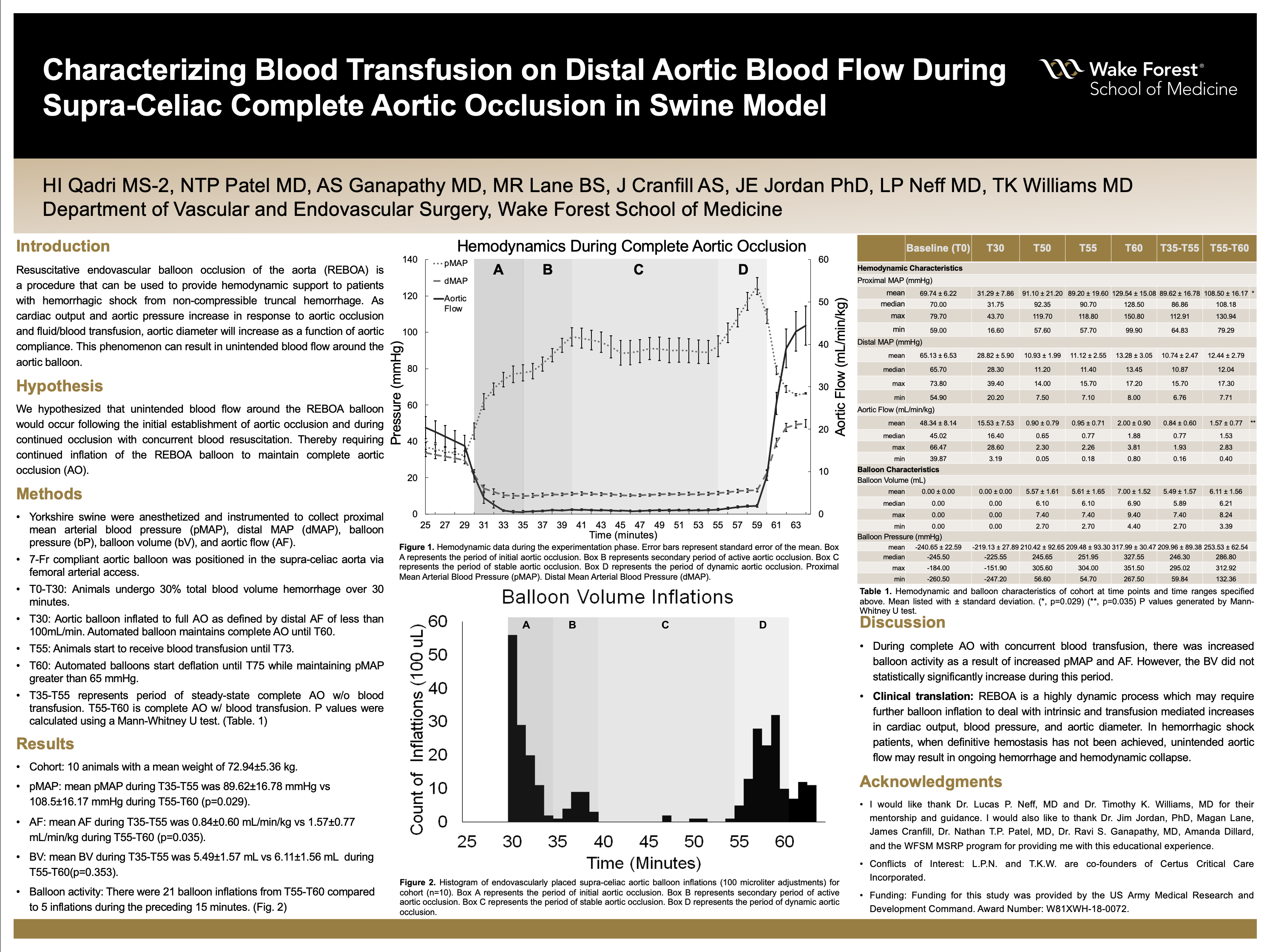
Background: Resuscitative endovascular balloon occlusion of the aorta (REBOA) is an endovascular procedure that can be used to provide hemodynamic support to hemorrhagic shock patients with non-compressible truncal hemorrhage. During REBOA, patients often receive blood transfusions to improve hemodynamics and correct hypovolemia before definitive surgical hemostasis. As cardiac output and aortic pressure increase in response to aortic occlusion and fluid and blood transfusion, aortic diameter will increase as a function of aortic compliance. This may result in unintended flow around the aortic balloon. To date, this leakage phenomenon has not been fully characterized and must be mitigated by progressive balloon inflation to maintain complete occlusion and to avoid ongoing hemorrhage.
Hypothesis: We hypothesized that unintended blood flow around the REBOA balloon would occur following the initial establishment of aortic occlusion and during resuscitation, requiring continued inflation of the balloon to maintain complete aortic occlusion (AO).
Methods: Yorkshire swine were anesthetized and instrumented to collect proximal mean arterial blood pressure (pMAP), distal MAP (dMAP), balloon pressure (bP), balloon volume (bV), and aortic flow (AF). A 7 Fr compliant aortic balloon was positioned in the supra-celiac aorta via femoral arterial access. Animals underwent 30% total blood volume hemorrhage over 30-min (T0-T30). At T30, the balloon was inflated to complete AO, defined by distal aortic flow of <100ml/min. Automated balloon inflation occurred from T30-T60 when downstream flow was detected. At T55, blood was transfused over 18-min (T55-T73). At T60, automated balloon deflation ensued to maintain a pMAP >65 mmHg over 15 minutes. P values were calculated using a Mann-Whitney U test.
Results: Hemodynamics were analyzed for 10 animals (weight 72.94±5.36 kg). At T30, T50, T55, and T60 the mean pMAP was 31.29±7.86 mmHg, 91.10±21.20 mmHg, 89.20±19.60 mmHg, and 129.54±15.08 mmHg. During complete AO and ongoing blood transfusion (T55-T60), mean pMAP was 108.5±16.17 mmHg and mean dMAP was 12.44±2.79 mmHg. The mean AF at T30, T50, T55, and T60 was 15.53±7.53 mL/min/kg, 0.90±0.79 mL/min/kg, 0.95±0.71 mL/min/kg, and 2.00±0.90 mL/min/kg. During steady state complete AO (T35-55) mean AF was 0.84±0.60 mL/min/kg. This increased statistically significantly to 1.57±0.77 mL/min/kg during T55-T60 (p=0.035). Mean bV at T30, T50, T55, and T60 was 0.00±0.00mL, 5.57±1.61 mL, 5.61±1.65 mL, and 7.00±1.52 mL. During steady state AO, mean BV was 5.49±1.57 mL, which increased to 6.11±1.56 mL (p=0.353) during AO with concurrent transfusion (T55-T60). The mean bP at maximum AO during blood transfusion was 253.53±62.54 mmHg. During T55-T60, there were 21 balloon inflations among the 10 animals analyzed compared to 5 inflations during the preceding 15-min of steady state AO.
Conclusions: Our data demonstrated that during REBOA with concurrent blood transfusion, progressive balloon inflation was required to maintain aortic occlusion due to increasing pMAP and AF. In clinical practice, following initial establishment of AO in the context of hemorrhagic shock, progressive balloon inflation may be required to maintain AO in response to intrinsic and transfusion mediated increases in cardiac output, blood pressure, and aortic diameter. This is particularly important when definitive hemostasis has not been achieved, as loss of aortic occlusion with blood flow beyond the balloon may result in ongoing hemorrhage and hemodynamic collapse.
Source of mentor’s funding or other support that funded this research: United States DoD and Dubie H. Holleman Fund for Cancer and Heart Research
-
Supporting Documents
- Characterizing Blood Transfusion on Distal Aortic Blood Flow During Supraceliac Complete Aortic Occlusion in Swine An...
Powered by Acadiate
© 2011-2024, Acadiate Inc. or its affiliates · Privacy
