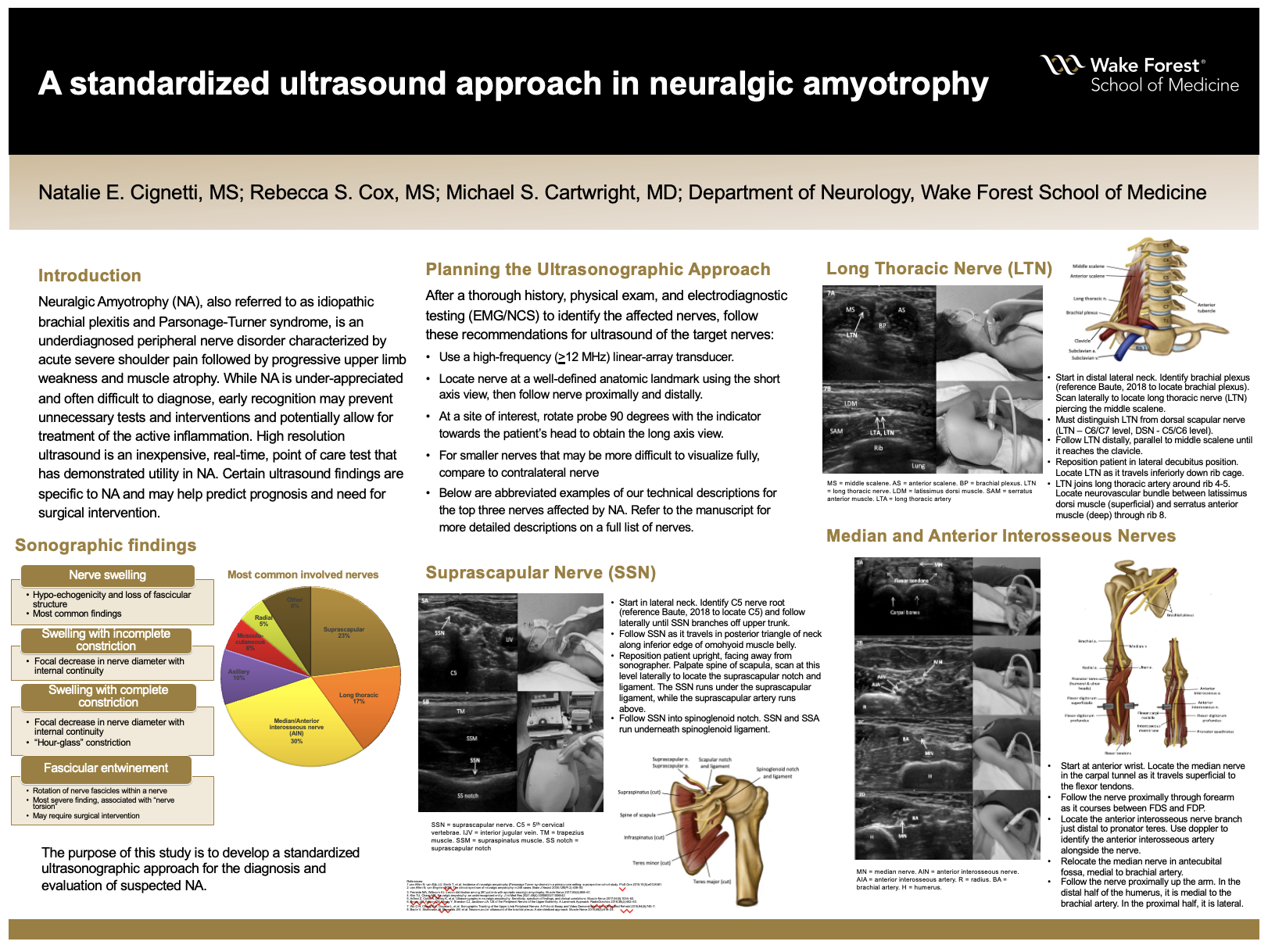
A standardized ultrasound approach in neuralgic amyotrophy
Poster Title: A standardized ultrasound approach in neuralgic amyotrophy
Student: Natalie Cignetti, Class of 2022; Siobhan Cox, Class of 2024
Faculty Mentor and Department: Michael Cartwright, MD, Neuromuscular, Neurology
ABSTRACT
Background: Neuralgic Amyotrophy (NA), also referred to as idiopathic brachial plexitis and Parsonage-Turner syndrome, is an uncommon peripheral nerve disorder characterized by acute severe shoulder pain followed by progressive upper limb weakness and muscle atrophy. NA likely has a multifactorial etiology and frequently involves specific nerves of the upper limb. While NA is under-appreciated and often difficult to diagnose, early recognition may prevent unnecessary tests and interventions, and potentially allow for treatment of the active inflammation. High resolution ultrasound is an inexpensive, real-time, point of care test that has demonstrated utility in NA. Certain ultrasound findings are specific to NA and may help predict prognosis and need for surgical intervention. The purpose of this study is to develop a standardized ultrasonographic approach for the diagnosis and evaluation of suspected NA.
Methods: Current literature was reviewed to determine appropriate recommendations to diagnose NA. We used a GE logic E ultrasound device and 12 MHz linear array transducer to image the nerves most frequently involved in NA on an ultrasound model. We first located each nerve near a well-defined anatomic landmark in the short axis view. From this site, we scanned proximally and distally along the entire length of the nerve or to the extent of which a reasonable image could be obtained. We saved images of each nerve at relevant locations throughout the neck and upper extremity. Anatomic reconstructions were created using Adobe Photoshop app to depict the relevant anatomy of each nerve course.
Results: Ultrasound images of the musculocutaneous, median, ulnar, radial, suprascapular, axillary, long thoracic, and phrenic nerves were obtained and displayed alongside photographs demonstrating probe location on an ultrasound model and anatomic reconstructions. Technical instructions on patient position, probe orientation, and how to locate and trace each nerve were described.
Conclusions: Our study describes a clinically relevant and feasible systematic approach for utilizing ultrasound as an adjuvant to history, physical exam, and electrodiagnostic testing in evaluating and diagnosing suspected NA.
 CLOSE SIDEBAR
CLOSE SIDEBAR