Complications following posterior total hip arthroplasty utilizing a piriformis-sparing posterior approach
Meckenzee Frank
Background: Total hip arthroplasty (THA) is one of the most performed elective procedures worldwide and is only expected to increase as the demographic shifts toward older age, and technology is allowing younger patients to have surgery. Since its development in the mid-20th century, many advancements have been made in surgical technique. The most common techniques used by practicing Orthopedists include the direct anterior approach (DAA), direct lateral approach (DLA), and the posterior approach (PA). Of these traditional approaches, only the DAA is considered to be muscle sparing between inter-nervous planes, while the DLA and PA involve muscle dissection. Our study describes complications following a minimally invasive piriformis-sparing posterior approach with an anatomic capsular repair. Muscle sparing techniques are typically described as having better outcomes and less complications, however, there is still debate about which THA technique is superior.
Hypothesis: Total hip arthroplasty completed by the senior author using the MIS piriformis-sparing posterior approach will have lower complication rates, both overall and for the specific complications, when compared to complication rates described in the literature for the traditional posterior approach, direct lateral approach, and direct anterior approach.
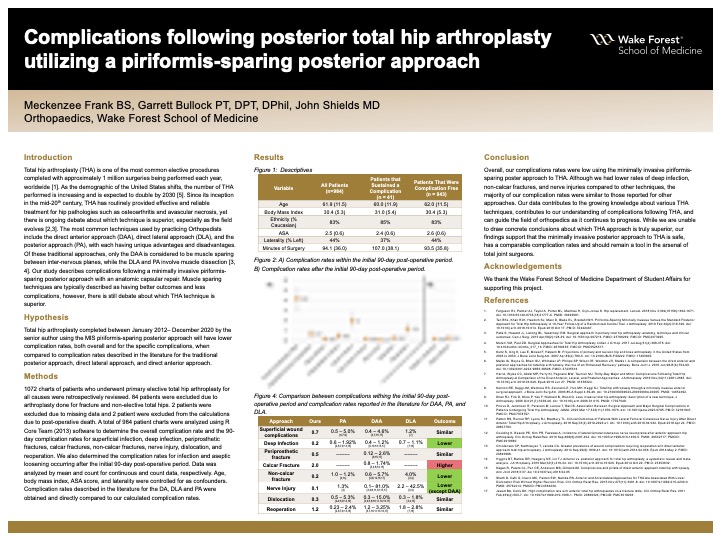
Methods: 1072 charts of patients who underwent primary elective total hip arthroplasty for all causes were retrospectively reviewed. 84 patients were excluded due to arthroplasty done for fracture, and non-elective total hips. A total of 984 patient charts were analyzed using R Core Team (2013) software to determine the overall complication rate and the 90-day complication rates for superficial infection, deep infection, periprosthetic fractures, calcar fractures, non-calcar fractures, nerve injury, dislocation, and reoperation. We also determined the complication rates for infection and aseptic loosening occurring after the initial 90-day post-operative period. Data was analyzed by mean and count for continuous and count data, respectively. Age, body mass index, ASA score, and laterality were controlled for as confounders. Complication rates described in the literature for the DA, DLA and PA were obtained and directly compared to our calculated complication rates.
Results: Overall complication incidence proportion over the 90-day post-operative period was 4.2%. The individual incidence proportions over this 90-day period were 0.7% for superficial infections, 0.2% for deep infection, 0.5% for periprosthetic fracture, 2.0% for calcar fracture, 0.2% for non-calcar fracture, 0.1% for nerve injury, 0.3% for dislocation, and 1.2% for reoperation. Following the initial 90-day period, two patients, 0.2%, sustained aseptic loosening and three patients, 0.3%, sustained infection. 2 patients sustained post-operative death. Our complication rates for superficial infection, periprosthetic fractures, dislocations and reoperations were similar to complication rates reported in the literature for other techniques. Our rate of deep infection was lower than the reported rates for other techniques. Our rate of calcar fractures was slightly higher than rates reported for the DAA. Our nerve injury rate was similar to that reported for DAA, but lower than the reported rates for DLA and PA.
Conclusions: Overall, our complications rates were low using the minimally invasive piriformis-sparing poster approach to THA. Although we had lower rates of deep infection compared to other techniques, the rates of other complications were similar to those reported for other THA approaches. Although we are unable to draw concrete conclusions about which THA approach is truly superior, our findings support that the posterior approach to the hip has a comparable complication rate and should remain a tool in the armamentarium for total joint surgeons.

