Your message has been sent.
 CLOSE SIDEBAR
CLOSE SIDEBAR
The Association Between Vitamin D and Hypertension-Related Heart Changes in Youth Referred for Hypertensive Disorders
Neema Moeini-Rastegar
Poster Title: The Association Between Vitamin D and Hypertension-Related Heart Changes in Youth Referred for Hypertensive Disorders
Student: Neema Moeini-Rastegar, Class of 2024
Faculty Mentor and Department: Andrew Michael South, MD, MS, Pediatric Nephrology
Funding Source: none
ABSTRACT
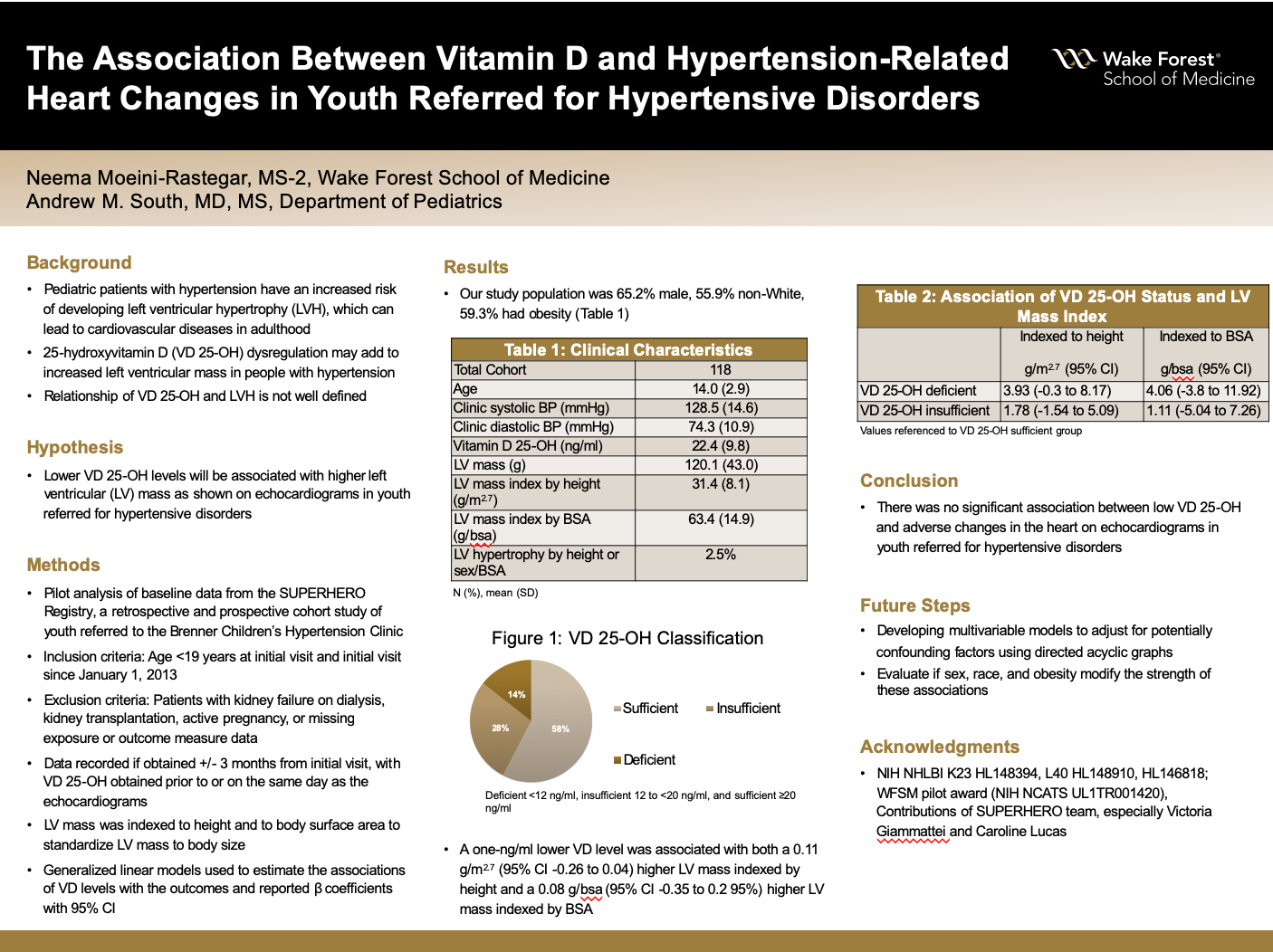
Background: Pediatric patients with hypertension have an increased risk of developing left ventricular hypertrophy (LVH), which could lead to cardiovascular diseases (CVD) later in adulthood. While the exact mechanisms contributing to LVH development are not fully understood, vitamin D (VD) dysregulation, including 25-hydroxyvitamin D (25-OH), may contribute to increased left ventricular mass in youth with hypertensive disorders, but this relationship has not been properly explored. The objective was to investigate whether low VD levels are associated with a higher risk of LVH in youth referred for hypertensive disorders.
Hypothesis: Lower VD 25-OH levels will be associated with the presence of LVH and an increase in left ventricular mass as shown on echocardiograms in youth referred for hypertensive disorders.
Methods: This is a pilot analysis of baseline data from participants enrolled in the Study of the Epidemiology of Pediatric Hypertension (SUPERHERO) Registry, a retrospective and prospective cohort study of youth referred for hypertensive disorders to the Brenner Children’s Hypertension Clinic. Study inclusion criteria were age <19 years at initial visit and initial visit since January 1, 2013. Patients with kidney failure on dialysis, kidney transplantation, or active pregnancy at the baseline visit were excluded; for this analysis, we additionally excluded participants who were missing exposure or outcome measure data. We recorded VD 25-OH and echocardiogram data if obtained +/- 3 months from date of first clinic visit. VD 25-OH must have been obtained prior to or on the same day as the echocardiograms. VD status was classified as sufficient (≥20 ng/ml), insufficient (12 to <20 ng/ml), or deficient (<12 ng/ml). Left ventricular mass was indexed to height (LVMI by height) and to body surface area (LVMI by BSA) to standardize left ventricular mass to body size. We used generalized linear models to estimate the associations of VD levels with the outcomes and reported β coefficients with 95% CI.
Results:Our study population was 65.2% male, 55.9% non-White, 59.3% had obesity, and the mean age was 14.0 years (SD 2.9). The mean VD 25-OH was 22.4 ng/ml (SD 9.8); 28.0% had insufficiency and 14.4% had deficiency. The mean LVMI by height and BSA were 31.4 (SD 8.1) ng/ml and 63.4 ng/ml (SD 14.9), respectively, and only 3 participants (2.5%) had LVH. A one-ng/ml lower VD level was associated with both a 0.11 g/m^2.7 (95% CI -0.26 to 0.04) higher LVMI by height and a 0.08 g/bsa (95% CI -0.35 to 0.2 95% CI) higher LVMI by BSA, though these were not statistically significant. Compared to being VD sufficient, individuals who were insufficient had a 1.78 g/m^2.7 (95% CI -1.54 to 5.09) higher LVMI by height and a 1.11 g/bsa (95% CI -5.04 to 7.26) higher LVMI by BSA, while those who were deficient had a 3.93 g/m^2.7 (95% CI -0.3 to 8.17) higher LVMI by height and a 4.06 g/bsa (95% CI -3.8 to 11.92) higher by BSA. However, these results were not statistically significant.
Conclusions:In this retrospective and prospective cohort study of youth with hypertensive disorders, we did not observe a significant association between low VD 25-OH and adverse changes in the heart on echocardiograms in youth referred for hypertensive disorders. Future steps include working on the multivariable models to adjust for potentially confounding factors, as well as evaluating how sex, race, and obesity may impact heart outcomes in hypertensive youth.
Source of mentor’s funding or other support that funded this research:
NIH NHLBI K23 HL148394, L40 HL148910, HL146818; WFSM pilot award (NIH NCATS UL1TR001420)
Powered by Acadiate
© 2011-2024, Acadiate Inc. or its affiliates · Privacy
