Your message has been sent.
 CLOSE SIDEBAR
CLOSE SIDEBAR
Perioperative Chemotherapy for Resectable Colorectal Liver Metastases: Analysis from the Colorectal Operative Liver Metastases International Collaborative
Rohin Gawdi
Background: Perioperative chemotherapy has been increasingly used with surgery as multimodality treatment for resectable colorectal-liver metastases (CLM). There is paucity of clinical data addressing optimal timing of chemotherapy administration relative to surgery.
Hypothesis: We examined outcomes of patients undergoing neoadjuvant and adjuvant chemotherapy in an international multicenter database of surgically-managed CLM.
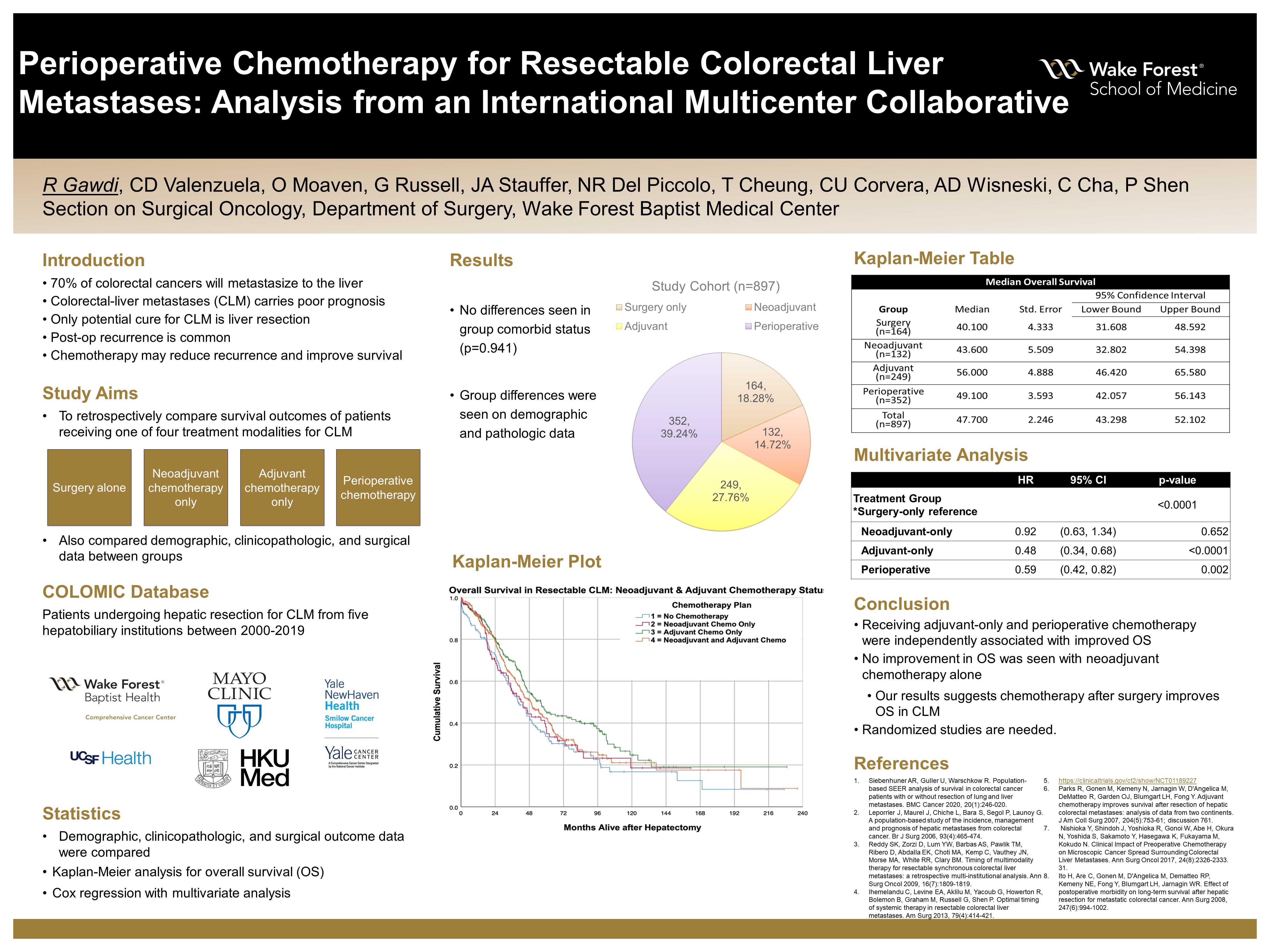
Methods: Data from 897 patients were obtained from a collaborative of CLM hepatectomy cases from five hepatobiliary institutions between 2000-2018. Overall survival (OS) was measured from time of hepatectomy for patients receiving: surgery alone, neoadjuvant chemotherapy, adjuvant chemotherapy, and neoadjuvant-plus-adjuvant chemotherapy. Kaplan-Meier analysis was performed to detect differences in OS between treatment groups. Single- and multi-variable analysis with Cox proportional hazards were run for OS between groups.
Results: 164 patients (18.28%) received surgery, 132 (14.72%) received neoadjuvant-only, 249 (27.76%) received adjuvant-only, and 352 (39.24%) received neoadjuvant-plus-adjuvant chemotherapy; with median OS of 40.1, 43.6, 56.0, and 49.1 months, respectively. Median OS for adjuvant-only was significantly longer compared to neoadjuvant-only (p=0.047) and surgery (p=0.004), and similar to neoadjuvant-plus-adjuvant (p=0.104). There were no significant differences in comorbidities between groups, based on Charlson-Deyo scores (p=0.941). There were significant differences in number of lesions (p<0.0001) and maximum tumor size (p =0.0008) between groups. On multivariate analysis, extrahepatic disease (p=0.0002), intraoperative transfusion (p<0.0001), number of lesions (p<0.0001), and treatment algorithm (p<0.0001) were independent predictors of OS.
Conclusions: Despite group differences, adjuvant chemotherapy for CLM was independently associated with improved OS compared to other chemotherapeutic approaches. For patients with resectable disease, upfront surgery should be considered.
Source of mentor’s funding or other support that funded this research: Department of Surgery
Powered by Acadiate
© 2011-2024, Acadiate Inc. or its affiliates · Privacy
