Your message has been sent.
 CLOSE SIDEBAR
CLOSE SIDEBAR
Machine Learning in Medicine: Predicting Total Hip Arthroplasty Surgical Outcomes
Robert Glover
Background: A total hip arthroplasty (THA) is a restorative surgery that greatly improves patients’ quality of life. Facing rising surgical demand for THAs, proper patient selection is critical to minimize postoperative complications and resource utilization and to optimize patient outcomes. Machine learning offers a potential solution by analyzing vast amounts of patient data to produce outcome predictions and patient risk profiles, allowing physicians to use clinical informatics as a supplement to their existing workflows for risk stratification.
Hypothesis: The study utilized data from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) to identify patient factors that predict the likelihood of postoperative infection, re-operation, and hospital readmission following THA. The proposed questions for each outcome of interest were:
1. What pre-surgical factors are the most predictive of a patient’s negative surgical outcome?
2. Can a clinically helpful model be developed utilizing several different machine learning techniques?
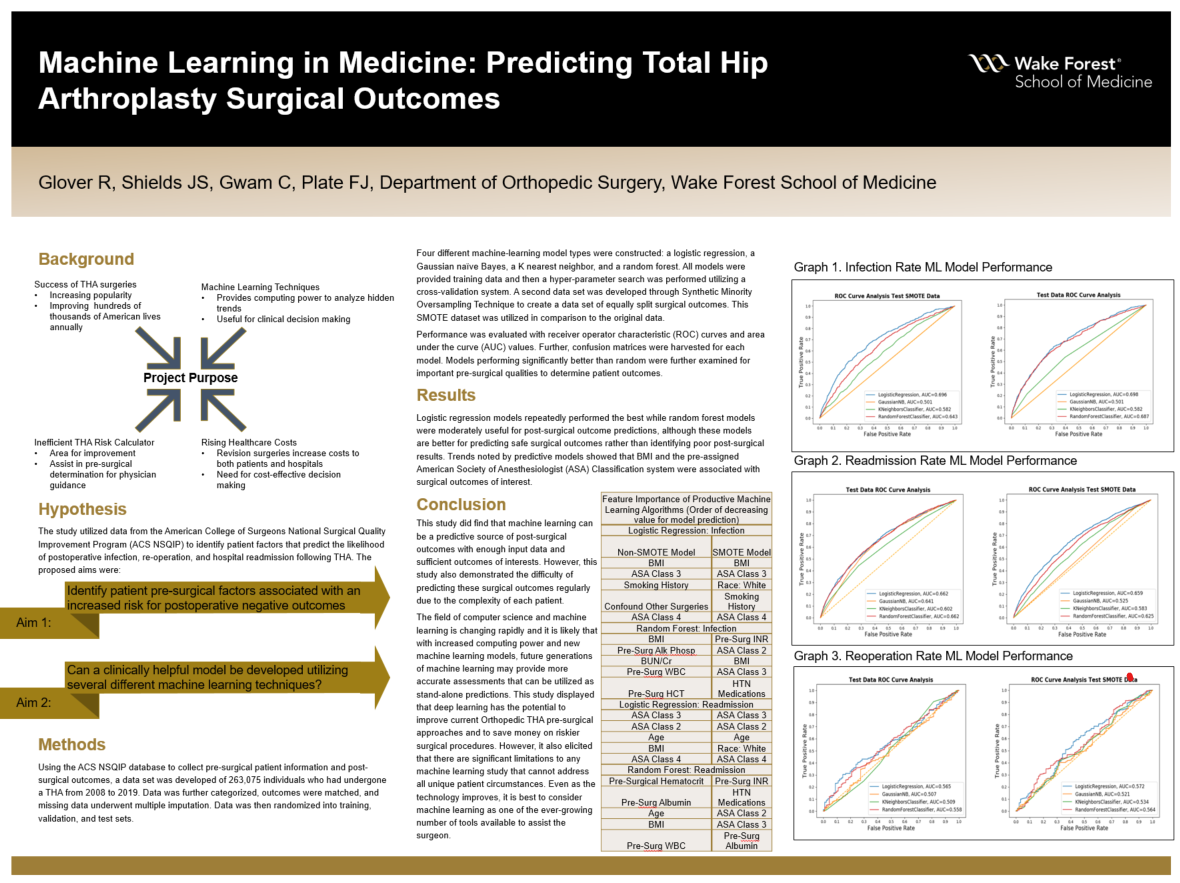
Methods: The ACS NSQIP database was used to retrieve pre- and post-operative patient information from individuals who had undergone THA between 2008 and 2019. Data analysis included data categorization, outcome matching, multiple imputations for missing data, and categorical encoding. Data was randomized and scaled into a training, validation, and test data set via a 70-15-15 split. Logistic regression, Gaussian naïve Bayes, K nearest neighbor, and random forest machine learning models were developed. Models were trained and a hyper-parameter search was performed utilizing a cross-validation system. Negative outcome rate prevalence was low in the training data set, so a second analysis was performed on an oversampled data set created through a Synthetic Minority Oversampling Technique (SMOTE) and compared with original data results. Test data was never altered. The performance of a model was estimated by receiver operator characteristic (ROC) curve and area under the curve (AUC) value. An AUC of 0.7 was determined as the threshold of a clinical meaningful model based upon an initial literature search before model development. Confusion matrices were harvested for each model. Models performing significantly better than random were examined for the important pre-surgical qualities impacting predicted outcomes.
Results: A total of 263,075 patients who had undergone THA were identified in the database. During model evaluation, logistic regression models repeatedly performed the best while random forest models were also moderately useful for post-surgical outcome predictions. These models were more accurate for predicting safe surgical outcomes. Trends noted by predictive models showed BMI, race, assigned American Society of Anesthesiologist (ASA) physical status classification, pre-surgical hematocrit, albumin, and INR were most predictive of THA postoperative negative outcomes.
Conclusions: As more patient data becomes available, a machine learning prediction model becomes a more realistic risk stratification tool that allows targeted patient selection for THA operations, minimizing the risk of complications. Machine learning tools further offer the ability to provide potential cost benefits, as expensive revision THA surgeries are often matched with prolonged hospital stays. The outcomes from such tools can be utilized by healthcare administrators and physicians as fiscal and patient outcome goals align to create effective pre-surgical screening predictions. Current machine learning models remain dependent on the data used for its validation, potentially leading to an over-prediction or underestimation of the actual patient risk and other fallacies that accompany large data set analysis. Yet, machine learning algorithms, in their current state, remain as an opportunity to adjunct current clinical evaluation and risk stratification based on cohort studies.
Powered by Acadiate
© 2011-2024, Acadiate Inc. or its affiliates · Privacy
