Your message has been sent.
 CLOSE SIDEBAR
CLOSE SIDEBAR
SBRT Versus Surgical Resection in Elderly Early-Stage Lung Cancer Patients: A Retrospective Review
Sarah Friday
Background: Surgical resection is the current standard of care for medically operable early-stage non-small-cell lung carcinoma (NSCLC). The median age of diagnosis for lung cancer is 71 years. Following surgical resection, elderly patients may potentially face an increased risk of complications. An alternative and less invasive treatment modality using radiation is Stereotactic Body Radiation Therapy (SBRT). Before the advent of SBRT, there were no alternatives that could provide similar levels of local control to surgery. In an elderly population, consideration of the risk versus benefit ratio of different treatments is of the utmost importance and SBRT may be preferred for elderly patients.
Hypothesis: (1) There is a significant difference in survival in early-stage NSCLC patients over the age of 65 that received definitive treatment with SBRT compared to surgical resection. (2) Any difference in time to definitive treatment has an impact on clinical outcomes.
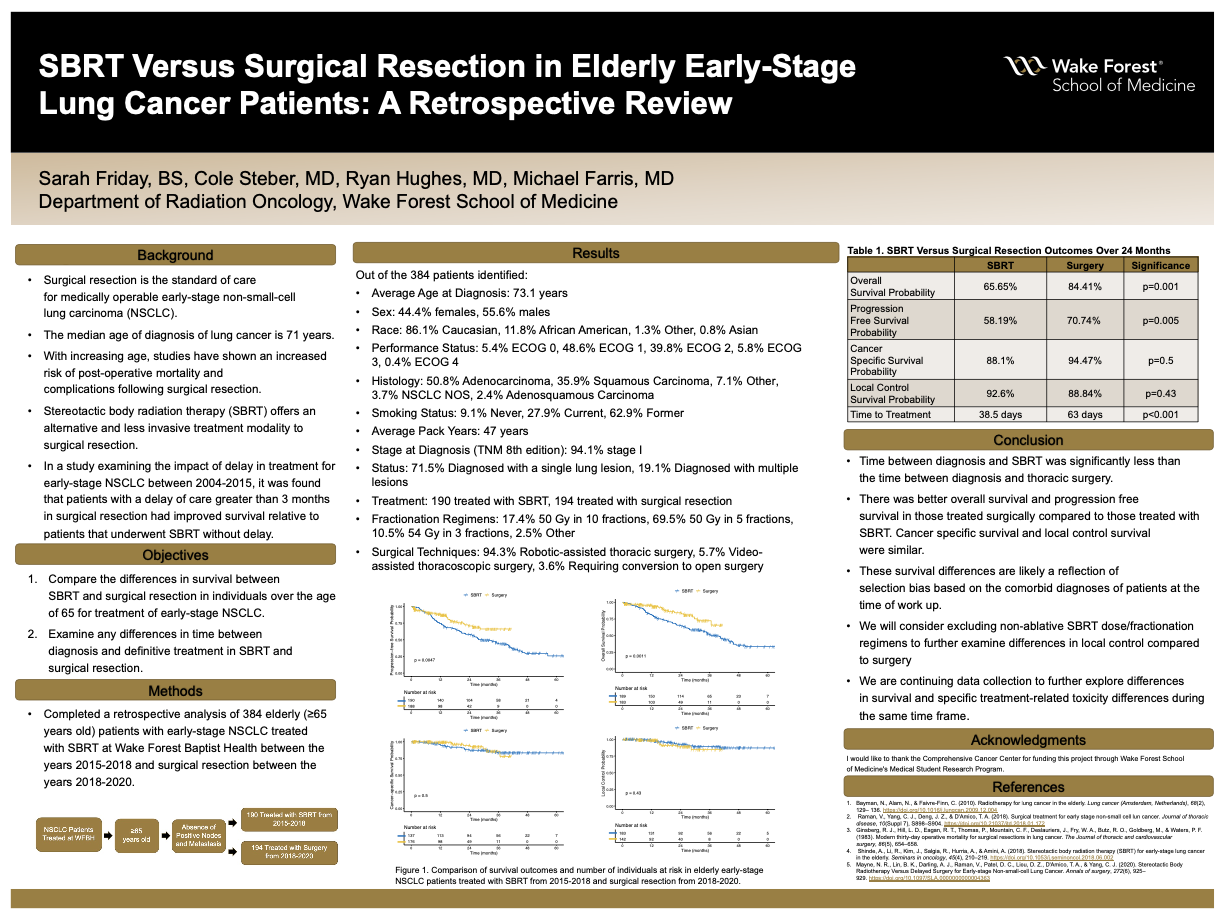
Methods: We retrospectively reviewed the medical records of elderly (≥65 years old) early-stage NSCLC patients treated with SBRT at Wake Forest Baptist Health between the years 2015-2018 and surgical resection between the years 2018-2020. Outcomes such as overall survival (OS), progression-free-survival (PFS), local control (LC), and cancer-specific survival (CSS) were analyzed using the Kaplan-Meier method and compared between cohort groups using the log-rank test.
Results: Of the 384 patients identified, all were ≥65 years old with the average age at diagnosis of 73.1 years, 213 (55.6%) were male, 190 were treated with SBRT and 194 with surgical resection. The majority of patients (71.5%) had an initial diagnosis of a single lung lesion, were stage I (94.1%) at diagnosis (TNM 8th edition), and a majority (86.7%) had a histology of adenocarcinoma or squamous cell carcinoma. Time to treatment was significantly different between treatment modalities with average days between diagnosis and treatment of 63 for surgical resection and 38.5 for SBRT (p<0.001). Various fractionation regimens were used for patients receiving SBRT including 50 Gy in 10 fractions (17.4%), 50 Gy in 5 fractions (69.5%), and 54 Gy in 3 fractions (10.5%). Various surgical techniques were utilized for patients in the surgical cohort, including robotic-assisted thoracic surgery (94.3%) with 7 patients (3.6%) requiring open conversion. In the 2 years following treatment, 16 (15.59%) surgical patients and 63 (34.35%) SBRT patients died. The 2-year OS was 84.41% and 65.65% for surgery and SBRT, respectively (p=0.001), while 2-year CSS was 94.47% and 88.1% surgery and SBRT (p=0.5). The 2-year PFS was 70.74% and 58.19% for surgery and SBRT, respectively (p=0.005). The 2-year LC was similar between the treatment modalities.
Conclusions: Time between diagnosis and SBRT was significantly less than the time between diagnosis and thoracic surgery. Despite this difference, for elderly patients undergoing surgery there was better OS and PFS compared to those treated with SBRT, while CSS and LC were similar. The survival differences likely reflect selection bias based on the comorbid diagnoses of patients at time of work up. We plan to continue exploring these preliminary results by analyzing patients treated during the same time period and further explore treatment related toxicity related to these treatment modalities in this elderly cohort with early-stage lung cancer.
Source of mentor’s funding or other support that funded this research: Department of Radiation Oncology.
-
Supporting Documents
- SBRT Versus Surgical Resection in Elderly Early-Stage Lung Cancer Patients: A Retrospective Review
Powered by Acadiate
© 2011-2024, Acadiate Inc. or its affiliates · Privacy
