Your message has been sent.
 CLOSE SIDEBAR
CLOSE SIDEBAR
Validation of Swallowing-related Organs at Risk in Patients Treated with Radiotherapy for Oropharyngeal Squamous Cell Carcinoma
Ankitha Iyer
Poster Title: Validation of Swallowing-related Organs at Risk in Patients Treated with Radiotherapy for Oropharyngeal Squamous Cell Carcinoma
Student: Ankitha Iyer, Class of 2024
Faculty Mentor and Department: Dr. Ryan Hughes, Radiation Oncology
Funding Source: Laura Scales Student Research Fellowship Fund
ABSTRACT
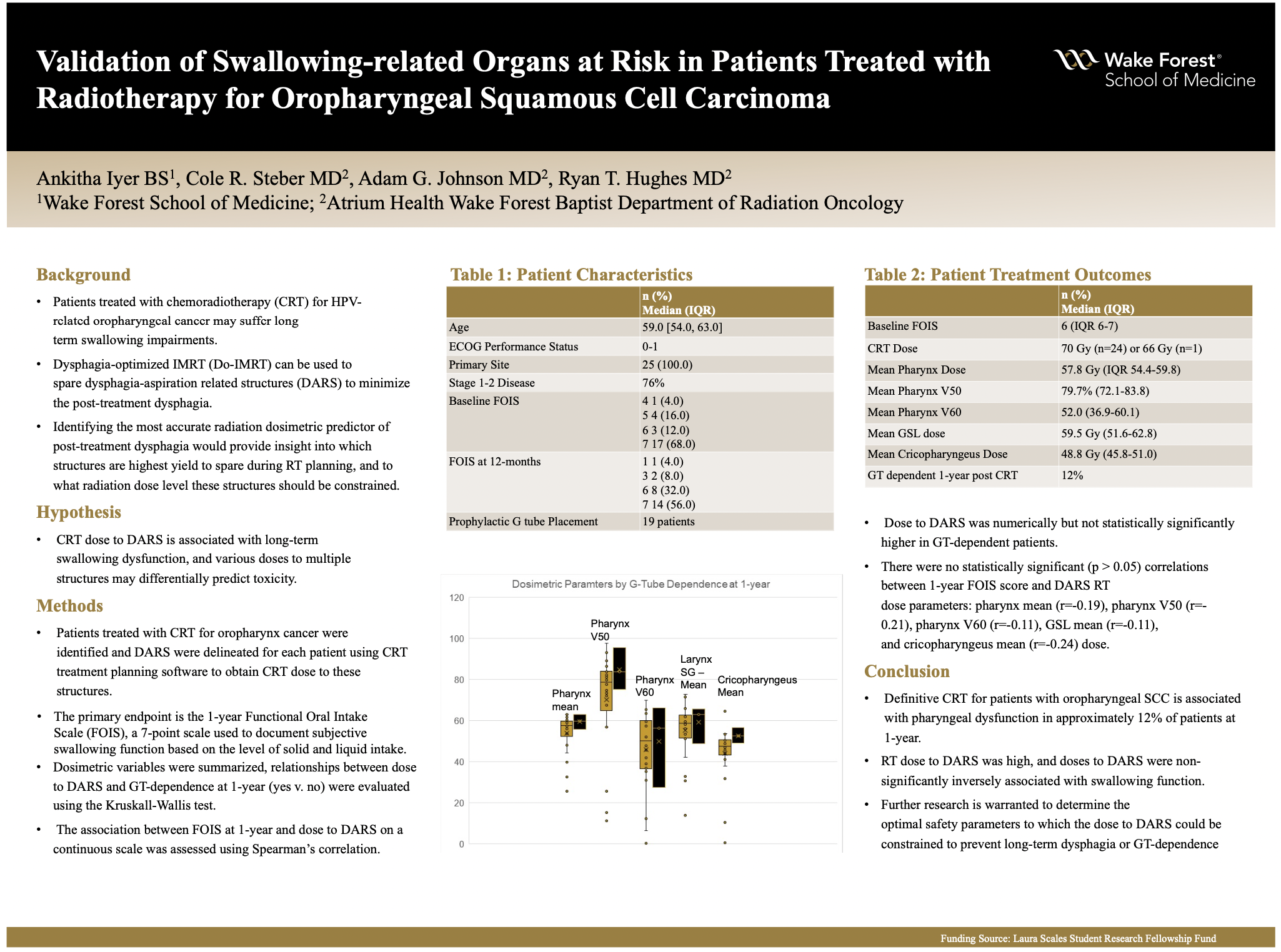
Background:Patients treated with chemoradiotherapy (CRT) for HPV-related oropharyngeal cancer may suffer long term swallowing impairments. Dysphagia-optimized IMRT (Do-IMRT) can be used to spare dysphagia-aspiration related structures (DARS) to minimize the post-treatment dysphagia. Identifying the most accurate radiation dosimetric predictor of post-treatment dysphagia would provide insight into which structures are highest yield to spare during RT planning, and to what radiation dose level these structures should be constrained.
Hypothesis:CRT dose to DARS is associated with long-term swallowing dysfunction, and various doses to multiple structures may differentially predict toxicity.
Methods:Patients treated with CRT for oropharynx cancer were identified and DARS were delineated for each patient using CRT treatment planning software to obtain CRT dose to these structures. The primary endpoint is the 1-year Functional Oral Intake Scale (FOIS), a 7-point scale used to document subjective swallowing function based on the level of solid and liquid intake. Dosimetric variables were summarized, relationships between dose to DARS and GT-dependence at 1-year (yes v. no) were evaluated using the Kruskall-Wallis test. The association between FOIS at 1-year and dose to DARS on a continuous scale was assessed using Spearman’s correlation.
Results:25 patients treated with CRT were included in the analysis. ECOG performance status was 0-1, 60% were current/former smokers, and 19 (76%) had Stage I-II disease. Prophylactic gastrostomy tube (GT) was placed in 19 patients. Median baseline FOIS was 6 (IQR 6-7). CRT dose was 70 Gy (n=24) or 66 Gy (n=1). Median of the mean pharynx dose was 57.8 Gy (IQR 54.4-59.8); median pharynx V50 and V60 were 79.7% (72.1-83.8) and 52.0 (36.9-60.1). Median of the mean GSL dose was 59.5 Gy (51.6-62.8) and median of the mean cricopharyngeus dose was 48.8 Gy (45.8-51.0). Three (12%) patients were GT-dependent at 1-year post CRT (1 with FOIS=1 and 2 with FOIS=3) and FOIS was 6-7 in the remaining 22. Dose to DARS was numerically but not statistically significantly higher in GT-dependent patients. There were no statistically significant (p > 0.05) correlations between 1-year FOIS score and DARS RT dose parameters: pharynx mean (r=-0.19), pharynx V50 (r=-0.21), pharynx V60 (r=-0.11), GSL mean (r=-0.11), and cricopharyngeus mean (r=-0.24) dose.
Conclusions:Definitive CRT for patients with oropharyngeal SCC is associated with pharyngeal dysfunction in approximately 12% of patients at 1-year. RT dose to DARS was high, and doses to DARS were non-significantly inversely associated with swallowing function. Further research is warranted to determine the optimal safety parameters to which the dose to DARS could be constrained to prevent long-term dysphagia or GT-dependence.
Source of mentor’s funding or other support that funded this research: Not applicable
Powered by Acadiate
© 2011-2024, Acadiate Inc. or its affiliates · Privacy
